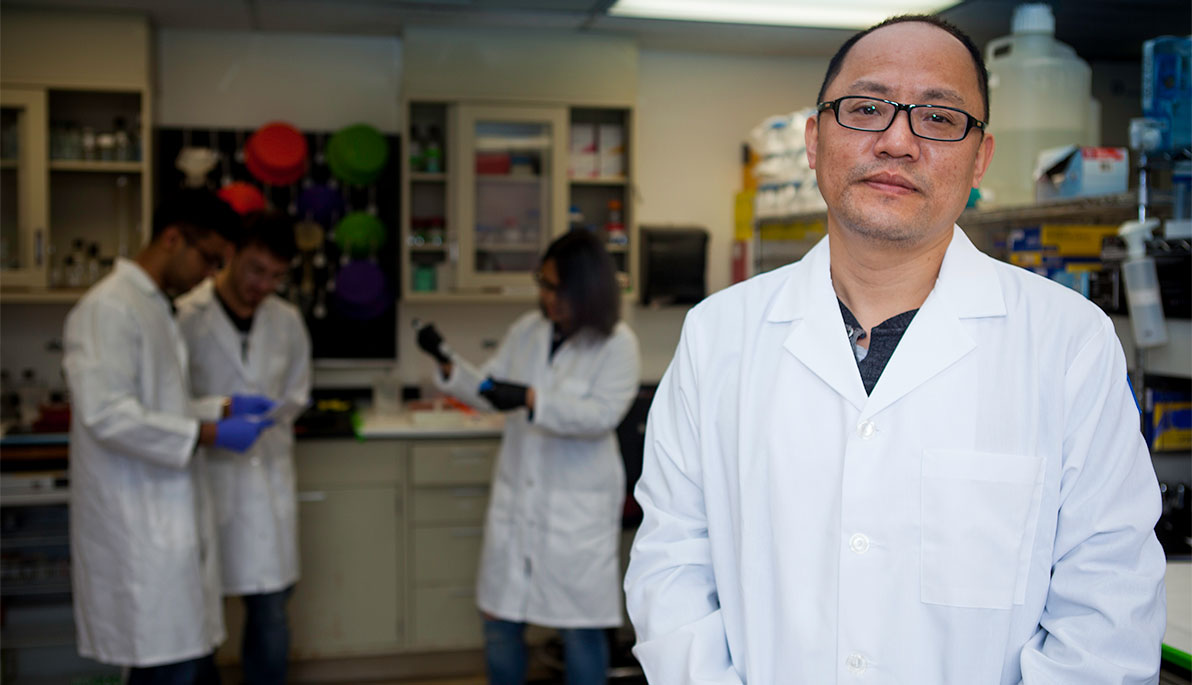
Faculty Profile: Haotian Zhao, Ph.D.
Title: Associate Professor
Department: Biomedical Sciences
Joined NYIT: 2018
Campus: Old Westbury
Fighting Pediatric Brain Tumors
Brain tumors are the most frequent cause of death from childhood cancers, and yet the ability to understand their origin and develop effective therapies has lagged compared to adult brain cancers. Over the past 20 years, only a few new drugs have been approved that were specifically developed to treat children with cancer.
Associate Professor of Biomedical Sciences Haotian Zhao, Ph.D., hopes to change that. With $1.7 million in grant funding from the National Cancer Institute (NCI), an arm of the National Institutes of Health (NIH), Zhao is conducting research on the choroid plexus tumor, a very rare, aggressive brain tumor that accounts for approximately 20 percent of brain tumors in children within the first year of life.
Because choroid plexus tumors are typically diagnosed in infants and young children, Zhao says it’s not clear if the tumors develop before or after birth. He’s attempting to understand how the molecular circuit of choroid plexus tumors interacts with signaling pathways as tumors are formed, with an ultimate goal to discover therapeutic targets for the development of safer and more effective therapies.
“This is a very rare disease with no established treatment protocol,” says Zhao, who relocated his lab from the University of South Dakota to NYIT College of Osteopathic Medicine (NYITCOM) in January 2018. “So when doctors see this, they typically treat it with a generic mix of chemotherapy, surgery, and radiation, which have lifelong debilitating complications for small kids if they even survive the disease.” Among these complications are hearing loss and the stunting of cell development as children age into adults—side effects that have been linked to chemotherapy.
One of the common malignant pediatric brain tumors is medulloblastoma, and Zhao initially focused his research on that type of tumor. But as with many scientific discoveries, his experiments led to a discovery about the choroid plexus tumor. While conducting research on medulloblastoma, Zhao developed an animal model to see what would happen if he used gene activation in the cerebellum. The surprising result was that the mouse subjects developed choroid plexus tumors that resembled human disease.
“Much of cancer research is conducted from human-derived materials. Because the choroid plexus tumor is so rare, there’s little systematic effort to derive these materials from human patients, so we are mostly reliant on the animal models to gain the understanding of the biology of the disease,” he says.
Because so little is known about the basis of choroid plexus tumors, Zhao realized he had the opportunity to enhance the medical field’s understanding of this lethal disease. His initial findings were published in Nature Cell Biology in 2016, and he subsequently received the NCI grant to fund further studies.
At NYIT, Zhao has engaged both undergraduate and medical students to work in his lab to gain experience with cancer research. In addition to inquiry on the choroid plexus tumor, Zhao continues his work to improve survival rates and treatments for children with medulloblastoma. “While the survival rate is much better, 15 to 20 percent of patients still die, typically from recurrence or metastasis of the disease away from the primary site,” he says.
Zhao has also developed a phenotype in animal models that mimics human disease to try and understand how the medulloblastoma cells migrate through cerebral spinal fluid to other areas of the brain or spinal cord. “If we can disrupt this kind of host and tumor cell interaction, perhaps we can disrupt the colonization of the tumor to other sites,” he says.
Ultimately, Zhao wants to better understand the biology of pediatric brain tumors to identify targets for innovative therapies that can specifically suppress tumor growth without damaging the developing brain. “The current treatments often aren’t successful, and when they are, they have devastating side effects,” says Zhao. “My hope is to develop better ways of treating these tumors based on their own biology.”









